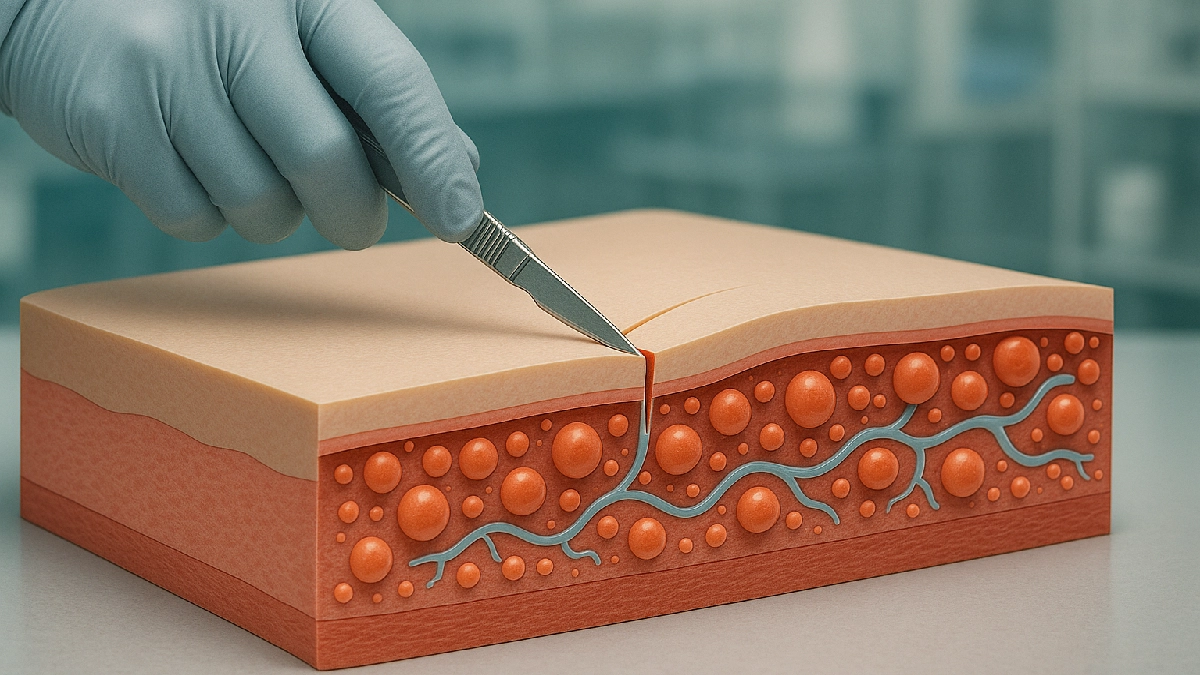
Imagine a training mannequin whose flesh feels like real human skin—one that bleeds slightly when cut and springs back under a scalpel. That’s the goal behind a recent breakthrough: researchers have developed 3D-printed simulated human tissue that mimics real body tissue to help doctors and surgeons train more realistically. This kind of innovation could reshape medical education and improve surgical outcomes.
Why It’s a Big Deal
In the past, surgical training often used static models, cadavers, or animal tissues. These have limitations in realism, cost, and ethical concerns. The new 3D-printed tissue depends on microcapsules that replicate fluid (like blood) and internal structural features, so when you cut it or press on it, it reacts more like real biological tissue. The method was reported by researchers at the University of Minnesota in a study published in Science Advances. (Science Advances article)
According to a university news release, the printed simulants matched directional strength, stretchiness, and softness more closely than earlier rigid models. ([University of Minnesota release](Researchers created 3D-printed simulated human tissue for medical training))
How It Works: The Tech Behind the Tissue
Think of the process like baking a layered cake—but at the micro scale, with fluids embedded:
- Design internal microstructures to control mechanical properties (softness, strength).
- Print microcapsules containing liquid (to simulate blood) without disrupting the structure.
- Layer the materials precisely so directional properties (how strong in one direction vs another) match real tissue.
- Test tactile feedback by having surgeons cut, suture, and feel the material.
One article from MedicalXpress describes how the team controlled internal patterns and added a formula to predict how the tissue behaves under pressure or cutting. (MedicalXpress coverage)
Surgeons in early trials rated these printed models higher in realism, particularly how the models respond when cut or pressed, compared with older simulant materials. (Newswise report) (Newswise)
Benefits for Medical Training
- Better realism = better muscle memory: Surgeons can practice more lifelike incisions and sutures.
- Ethical & scalable: Reduces reliance on animal or cadaver tissue.
- Customizable: You could one day print models of a patient’s own tissues for practice.
- Cost efficiency over time: Though initial costs are high, reusable and consistent models may reduce long-term training expense.
Challenges & What Comes Next
- Scaling up: Printing full organs or large tissue sections is still hard.
- Cost & speed: The more complex the model, the more expensive and slower its production.
- Durability: The simulants must handle repeated cuts, sutures, and manipulation.
- Tool compatibility: They need to respond well to surgical tools like electrocautery (heat) or lasers.
Next steps include printing varied organ shapes, testing with different surgical tools, and integrating feedback loops so the model “reacts” to different techniques.
Frequently Asked Questions (FAQs)
Q1: Does this “fake tissue” actually bleed?
Yes — the microcapsules contain fluid to simulate bleeding behavior when cut, improving realism.
Q2: Are these models safe for students to practice on?
Yes. They are non-biological, sterile, and manufactured in labs—no risk of infection or disease transmission.
Q3: When might this become widely used?
While prototypes exist now, adoption in medical schools and hospitals could take several years as costs and printing speed improve.
Conclusion
This 3D-printed simulated tissue marks a leap forward in how medical professionals can train. By combining fluid dynamics, precise structure, and biomechanical behavior, it bridges the gap between synthetic models and living flesh. As technology matures, we may see surgeons practicing on replicas of a patient’s own organs before actual surgery.
Key Takeaway: These innovations promise safer, more effective training—and the possibility of personalized surgical models in the near future.
Last Updated on October 18, 2025 by Lucy